Time to seriously consider focused mris for injured spines
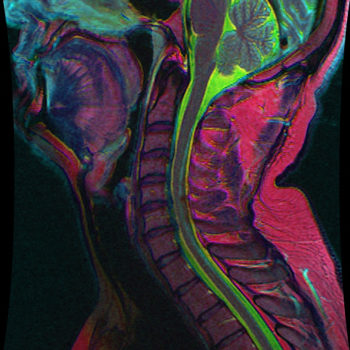
Is it sufficient to only examine the injured part of the spine via focused magnetic resonance imaging (FMRI) or will that lead to missed problems?
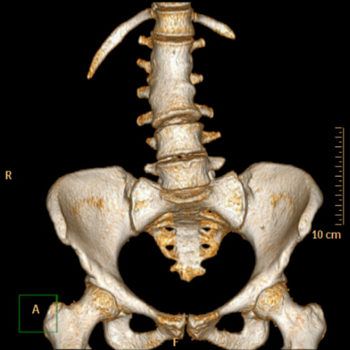
In patients who sustain blunt trauma, CT is the initial screening modality of choice in most emergency departments in the United States to look for injury to various parts of the body—including the spine. If a fracture is seen in the thoracic or lumbar spine on CT, sometimes an MRI of the injured segment of the spine is useful to provide additional information about the injury to help physicians decide on a treatment plan.”
“The problem is that MRI is a relatively expensive and time-consuming test compared to CT, so every time we were ordering MRIs of the entire spine in this scenario, it seemed somewhat excessive. Since we are mostly interested in looking at the part of the spine that we already know is injured (based on the CT), we asked ourselves if just imaging the injured portion of the spine by MRI (a focused MRI) would be adequate to provide the information we need to decide on a treatment plan. The concern with this approach is whether we would miss injuries by not looking at the entire spine by MRI.”
To answer the question, the investigators reviewed records for all adult trauma patients who presented to Mass General’s emergency department between 2008 and 2016 with one or more fractures of the thoracic and/or lumbar spine—as identified using computed tomography (CT) and who underwent MRI of the entire thoracic and lumbar spine within 10 days.
The most important result of the test, said Dr. Karim, was “that performing a focused MRI of only the injured portion of the spine would lead physicians to missing some sort of injury in another portion of the spine about 15% of the time, but none of these ‘missed injuries’ would lead to any change in treatment plan or patient care if they are known.”
“This is a very practical study from our perspective because it affects the day-to-day work of radiologists, emergency room physicians, and spine surgeons. If they see a fracture in the thoracic or lumbar spine on CT that they want to better characterize on MRI, they should be comfortable obtaining just a focused MRI of the injured portion of the spine—saving time, money, and patient discomfort.”
Reference From : https://ryortho.com