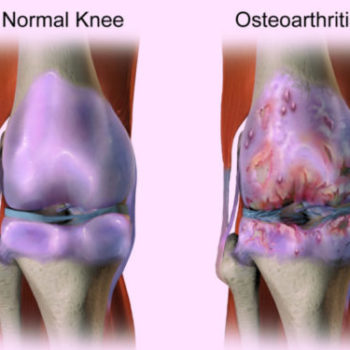
Efficacy and tolerability of duloxetine in patients with knee osteoarthritis
Researchers assessed the effectiveness and tolerability of duloxetine in patients with knee osteoarthritis (OA), one of the most common joint diseases. Data from six randomized controlled trials were pooled, including 2059 participants. According to findings, duloxetine is effective in managing chronic pain and physical function loss in knee OA with acceptable adverse events despite having no advantage in the treatment of joint rigidity.
Read the Full Article On :
In MDLinx (A meta-analysis of randomized controlled trials)