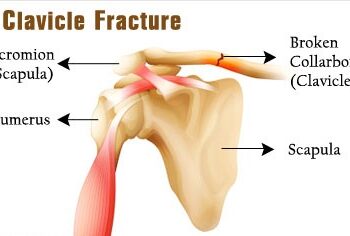
Clavicle Fracture
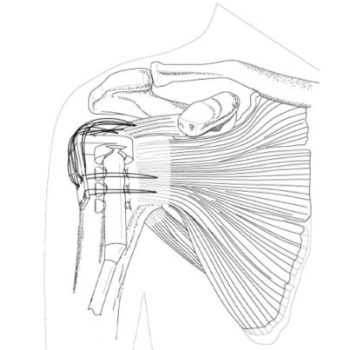
Anatomy
The clavicle is located between the ribcage (sternum) and the shoulder blade (scapula). It is the bone that connects the arm to the body.
The clavicle lies above several important nerves and blood vessels. However, these vital structures are rarely injured when a fracture occurs.
Clavicle fractures are fairly common and occur in people of all ages. Most fractures occur in the middle portion, or shaft, of the bone. Occasionally, the bone will break where it attaches at the ribcage or shoulder blade.
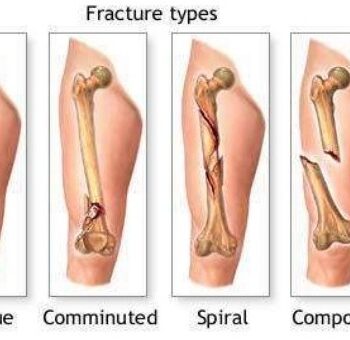
Clavicle fractures vary. The bone can crack just slightly or break into many pieces (comminuted fracture). The broken pieces of bone may line up straight or may be far out of place (displaced fracture).
Cause
Clavicle fractures are most often caused by a direct blow to the shoulder. This can happen during a fall onto the shoulder or a car collision. A fall onto an outstretched arm can also cause a clavicle fracture. In a baby, a clavicle fracture can occur during the passage through the birth canal.
Symptoms
A clavicle fracture can be very painful and may make it hard to move your arm. Other signs and symptoms of a fracture may include:
- Sagging of the shoulder downward and forward
- Inability to lift the arm because of pain
- A grinding sensation when you try to raise the arm
- A deformity or “bump” over the break
- Bruising, swelling, and/or tenderness over the collarbone