Tag Archives: Spine
- Home
- Posts tagged: Spine
Spine
You know what is Minimally Invasive Spine Surgery?

Written by(Full Credit) Benjamin T. Bjerke, MD, MS...
What are the Most Common Types of Orthopedic Surgery?

An orthopedic surgery is any operation performed o...
The role of malnutrition in 90-day outcomes after total joint arthroplasty

Via a cohort study of 4,047 cases, the researchers...
Efficiency of platelet-rich plasma therapy in knee osteoarthritis does not depend on level of cartilage damage

Platelet-rich plasma (PRP) is a concentrate of aut...
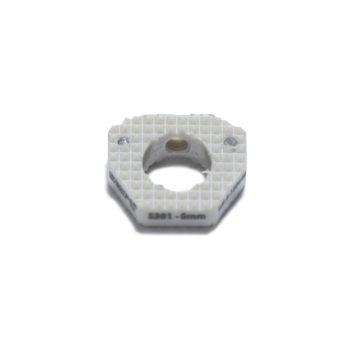
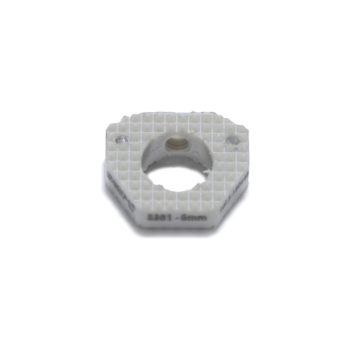
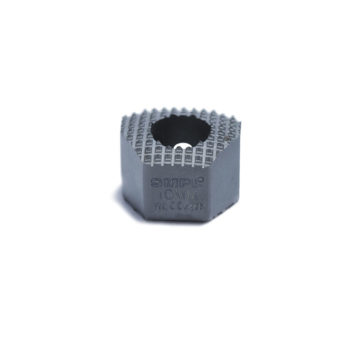
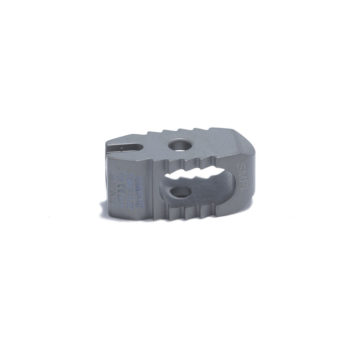
Orthopedic Implants to Dominate the Global 3D Printed Medical Devices Market

Increasing prevalence of chronic diseases and risi...







You know what is Minimally Invasive Spine Surgery?
Written by(Full Credit) Benjamin T. Bjerke, MD, MS...
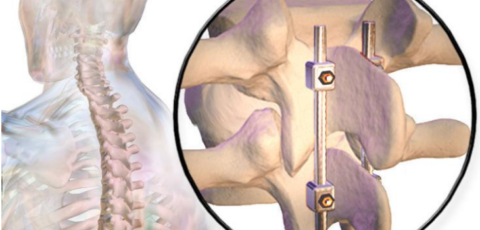
Postoperative Care for Spinal Fusion Surgery
The extended healing period required after lumbar...

What are the Most Common Types of Orthopedic Surgery?
An orthopedic surgery is any operation performed o...
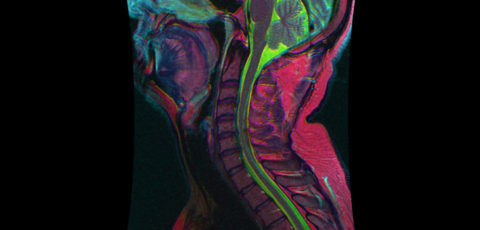
Time to seriously consider focused mris for injured spines
Is it sufficient to only examine the injured part...