Home Page
Welcome to Smit Medimed Pvt. Ltd.
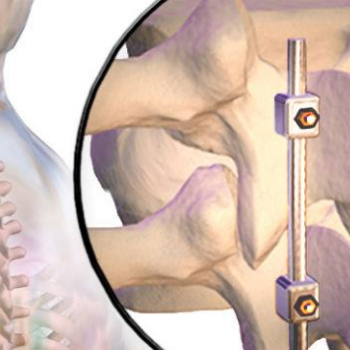
Established in the year 1990, Smit Medimed Pvt Ltd (SMPL) specializes as CDSCO certified Orthopedic Implants Producer & Exporter. We offer a wide variety of safe and advanced Orthopedic Implants and fixators. SMPL is a leading manufacturer and exporter of orthopaedic implants. SMPL have got a sound and firm position in the orthopedic industry by having a sturdy network of distributors domestically & around the globe.
Get Ready For Upcoming Event
ARAB HEALTH 2023
DUBAI
Product Categories

We are worldwide
We have created significant domestic, as well as global presence through our strategically placed distribution network.
- India
- Africa
- Europe
- Middle East
- Far East
- Brazil