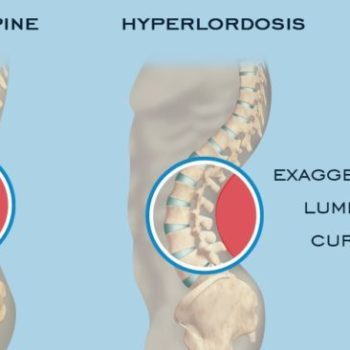
Lumbar Hyperlordosis
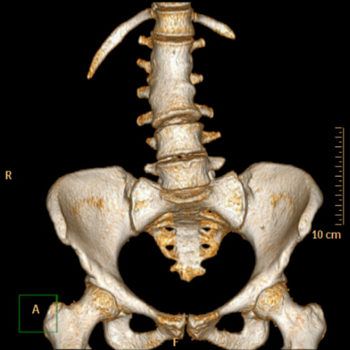
Lumbar lordosis refers to the inward curvature of the lumbar spine that is created by wedging of both the lumbar intervertebral discs and the vertebral bodies.
Deviations of the lumbar spine such as an increased lumbar lordosis have an impact on overall postural stability particularly in maintaining sagittal balance due to a degeneration of the sagittal spine curvature.
A greater lordosis angle is a risk factor for developing spondylolysis and ventral bulging of the affected vertebra, with researchers having proved a positive association between lumbar hyperlordosis angle and spondylolysis and isthmic spondylolisthesis.
Been and Kalichman gave a detailed description of the anatomy of lumbar lordosis stating that dorsal wedging of the vertebral bodies and discs increases the lordosis angle, whereas more ventral wedging of these structures reduces the lordosis angle ……………. Continue reading on mass4d.com: Lumbar Hyperlordosis
Copyright 2018 MASS4D® All rights reserved. This article or any portion thereof may not be reproduced without the prior written permission of MASS4D®